10 years ago, in January 2010, the New York Times started a series of articles about accidental overexposures in radiation therapy treatments. This milestone prompted us to consider the challenges Medical Physicists have experienced over the last 10 years and what kind of measures have been taken to improve patient safety in today’s radiation therapy processes.
We invited Marlies Pasler, Ph.D., Medical Physicist at Lake Constance Radiation Therapy in Friedrichshafen, Germany, to share her view on improving patient safety with us.
Improving patient safety – A Medical Physicist’s perspective
Over the past 10 years, patient safety has evolved in parallel with radiotherapy treatment techniques. It seems not so long ago that IMRT replaced 3DCRT and made pre-treatment verification measurements obligatory. The advent of highly conformal IMRT techniques was facilitated by IGRT procedures that allow increasingly precise patient positioning. Margins around the planning target volume decreased and the need for more accuracy in imaging, patient positioning and dose deposition increased.
“Phantom-based QA systems are time consuming and exhaustive to clinical staff”
Treatment plan complexity of highly modulated radiation therapy techniques require verification methods that ensure that the dose is delivered exactly as planned. Highly modulated treatment plans are therefore not only a challenge for treatment planning systems and linear accelerators, but also for dose measurement devices. Accordingly, complex measurement systems were developed and introduced to clinical routine. However, these phantom-based QA systems proved time-consuming and exhaustive for staff members. Logistically, plan verification could not always be provided before the first treatment fraction. Recently, phantom-less, automated and online plan verification methods have been developed. The most beneficial of these provide both complex dose verification and comprehensible evaluation, such as a single-ion chamber transmission detector that delivers online and real-time treatment verification.
“Enabling dose verification while the patient is being treated”
Emerging adaptive radiotherapy techniques have demanded not only fast and accurate treatment planning but also new solutions for treatment plan verification. For offline-adaptive radiotherapy, fast and reliable plan verification is needed. From this perspective, phantom measurements are too time-consuming as linac time is limited. Phantom-less, online approaches such as transmission detectors, log file evaluation and portal imaging dosimetry require no exhaustive phantom setup and thus enable dose verification while the patient is being treated.
Online-adaptive techniques require re-planning and dose verification while the patient is still on the treatment couch. Typically, second-check monitor unit calculation evaluates the accuracy of dose calculation. Beyond that, methods are needed to verify that the treatment machine delivers the plan as calculated. Hence, online plan verification methods, that can compare planned and delivered dose while the patient is being treated, are required.
“Systems that operate without user interaction further increase patient safety”
Since most errors are human-related, systems that operate without user interaction can further increase patient safety. For instance, using a fully automated system avoids potential disorders concerning the correct assignment of planned vs. delivered treatment plan for plan verification.
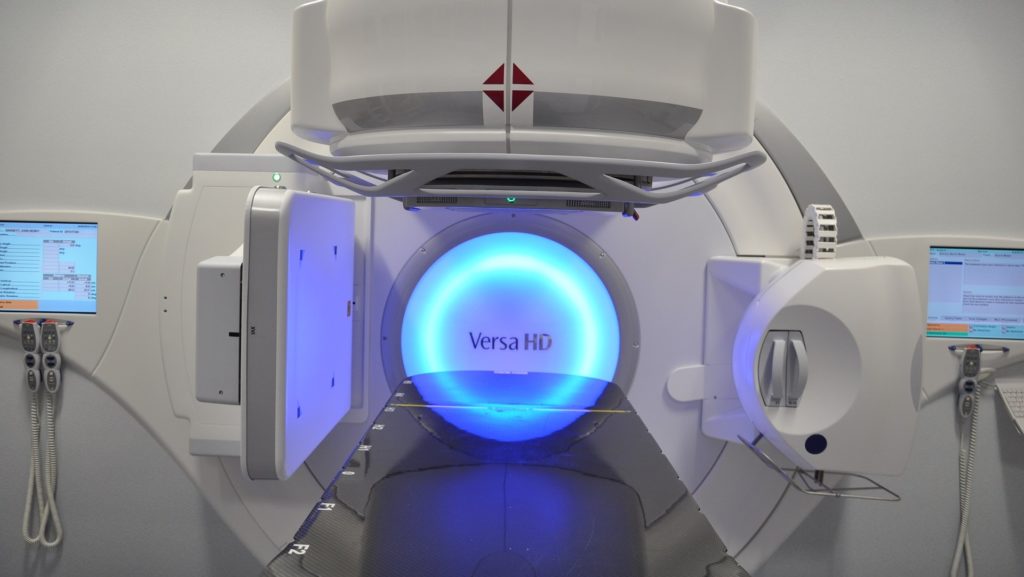
Dr. Marlies Pasler using IQM at the Elekta Versa HD Linear Accelerator
“Improving patient safety with online dose monitoring “
As real-time dose verification has become simple, fast and reliable, online dose monitoring for each fraction increases patient safety even more. These days, modern technology provides dose verification and monitoring that take place in the background. Such tools allow medical staff to focus on the aspects that matter most, such as patient well-being.
Patient safety is a primary focus in radiation therapy, where automated real-time dose measurement can help improve efficiency and efficacy. A clear-cut example is the way Dr. Pasler’s clinic employs IQM to monitor every patient’s treatment, every day, without additional staff effort.
If you would like to learn how IQM can help you to improve the safety of your patients please click here to visit the IQM website.
